In healthcare revenue cycle management (RCM), nothing stings more than watching hard-earned reimbursements vanish into the accounts receivable (AR) black hole. This rings especially true for payer denials that never get overturned, despite several attempts.
At a time when providers are already navigating seismic policy shifts (think Medicaid cuts under OBBBA and UHC’s anesthesia reimbursement reductions) and battling the twin pressures of rising costs and staffing shortages, poor RCM appeal and denial management can further derail revenue recovery if not worked with absolute precision.
Did you know?
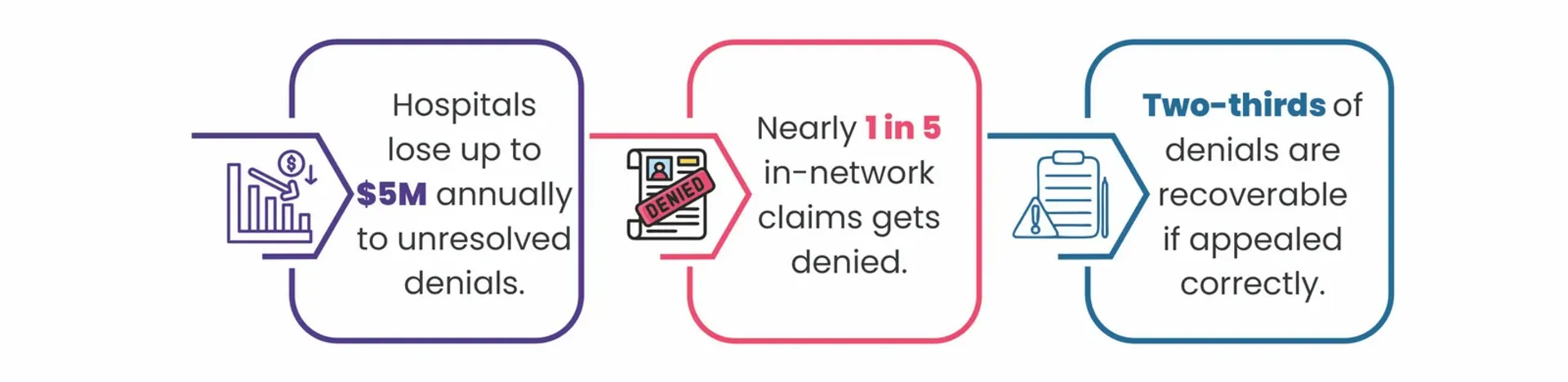
Going by the industry narrative, hospitals continue to lose millions annually to unresolved claim denials. Yet, studies consistently show that most denials are recoverable if appealed correctly.
Thus, proactive denial prevention and appeal management are your best bet to safeguard your revenue. Interestingly, most appeals fail not because the denial is justified but because the appeal process itself is flawed or weak.
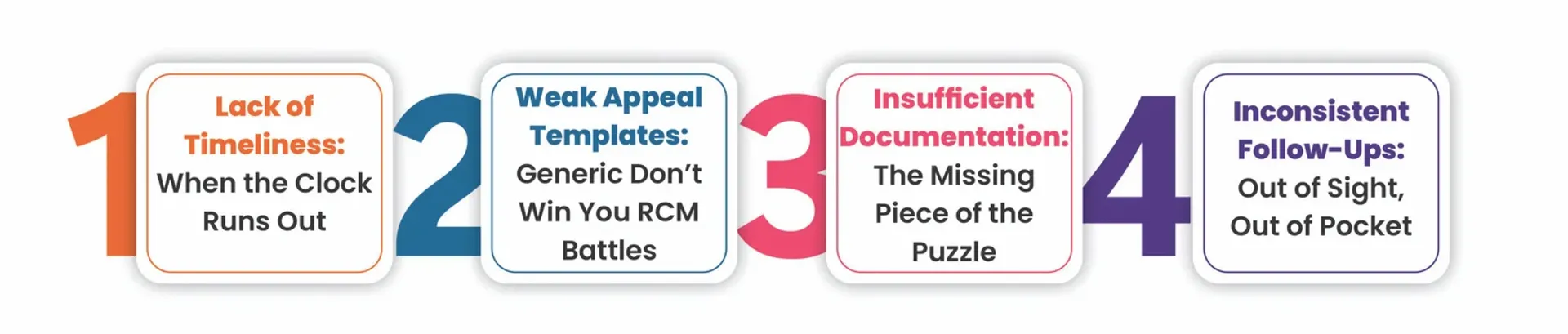
As an AI-enabled RCM services provider, we at Jindal Healthcare often see self-inflicted gaps in appeals that sabotage AR management and revenue recovery efforts of healthcare providers:
Lack of Timeliness: When the Clock Runs Out
Timeliness is everything in healthcare and an even more critical component of RCM. From front-end eligibility verification and prior authorizations to denial and appeal management (if, heaven forbid, it reaches that stage), time sensitivity is at the heart of all RCM functions.
RCM teams often hustle round the clock to keep pace with payers, who often enforce strict and varying deadlines for claims and appeal submissions. And missing these deadlines essentially means losing revenue that’s rightfully earned but not rightly claimed.
We often see providers with a backlog of aged claims, mostly still recoverable on paper, losing money because their appeal filing window had slammed shut.
How to Fix This
Implement SOP-driven, AI-powered RCM workflows that can flag denials in real time and route them for action based on urgency and payer timelines. Additionally, AI in RCM can triage accounts, so high-value, high-impact winnable claims are prioritized first with expert oversight to boost the appeal success rate and reduce AR aging.
Weak Appeal Templates: Generic Ones Don’t Win You RCM Battles
As a revenue cycle leader or healthcare CFO, you already know that a “one-size-fits-all” appeal template rarely convinces a payer. Appeals that read like boilerplate letters often fail to establish the medical necessity and compliance grounds needed to overturn denials.
Generic appeals in RCM, no matter how timely filed, rarely succeed if they lack a payer-specific nuance for dispute. Weak templates often ignore payer requirements and lack the clinical depth it takes to make a compelling case. When appeal templates aren’t tailored or supported by the right data, they stand a high chance of being dismissed by payers and an even higher chance of being written off.
How to Fix This
Develop payer-specific SOPs and appeal templates that adapt quickly while still grounded in clinical evidence and policy nuance. Effective appeals demand precision: referencing payer language, policy nuances, and medical necessity evidence. Without this, even the best denial management strategies can collapse at the finish line, wasting your revenue recovery efforts.
Insufficient Documentation: The Missing Piece of the Puzzle
Even your strongest argument can fall flat without adequate documentation to back it up. Most often, missing prior authorizations, incomplete medical records, or lack of clinical justification are the key reasons payers uphold denials and dismiss appeals.
Insufficient documentation remains one of the costliest pitfalls in RCM appeal management. The strength of an appeal depends on the quality and completeness of its supporting documentation: clinical notes, coding explanation, payer correspondence, and prior authorization proofs.
Yet, in many hospital settings, especially the rural ones that are often resource-strapped, we have seen information living in silos (EHRs and paper files) and appeals inconsistently formatted or missing critical medical necessity proofs.
This lack of cohesiveness in documentation often weakens the appeal narrative for hospitals, ultimately costing them their revenue. Even when the service is medically necessary, incomplete documentation provides payers grounds to uphold the denial, further delaying reimbursements or causing permanent revenue loss and wasted staff effort for hospitals.
How to Fix This
With AI-driven documentation review and expert oversight, you can move from reactive denial management to proactive revenue recovery assurance. When every appeal is validated at the source, supported by AI-driven contextual intelligence and expert-led documentation, the chances of revenue recovery increase manifold.
Inconsistent Follow-Ups: Out of Sight, Out of Pocket
Submitting a timely appeal is only half the battle won; consistent follow-ups are what turn potential recoveries into actual dollars. Delayed or inconsistent follow-ups on appeals rank among the top reasons for revenue leakage in the RCM process.
When claims sit far too long unattended after submission, often due to poor tracking or prioritization, chances are invariably high that your revenue will slip through the cracks.
Every missed follow-up window compounds the risk of preventable revenue loss. For many rural hospitals, where every dollar matters, inconsistent follow-ups often translate directly into prolonged AR cycles and cash flow risks.
As an AI-enabled RCM services provider, we often see CFOs admitting that they lost revenue not because they didn’t file appeals but because they didn’t follow up consistently.
How to Fix This
Adopt a structured follow-up cadence supported by appeal escalation workflows to keep your revenue on track. Monitor payer response times and behavior and track high-risk claims with AI automation. Leverage expert oversight to ensure timely escalation, root-cause analysis, and documentation accountability for every touchpoint. With AI-driven, expert-led RCM, no claim is ever really “out of sight.”
This synchronized blend of AI workflows and human intelligence transforms RCM appeal follow-ups into a revenue recovery engine, reducing AR aging, accelerating collections, and protecting revenue.
Moving Beyond Appeals to Building a Denial Prevention-First RCM
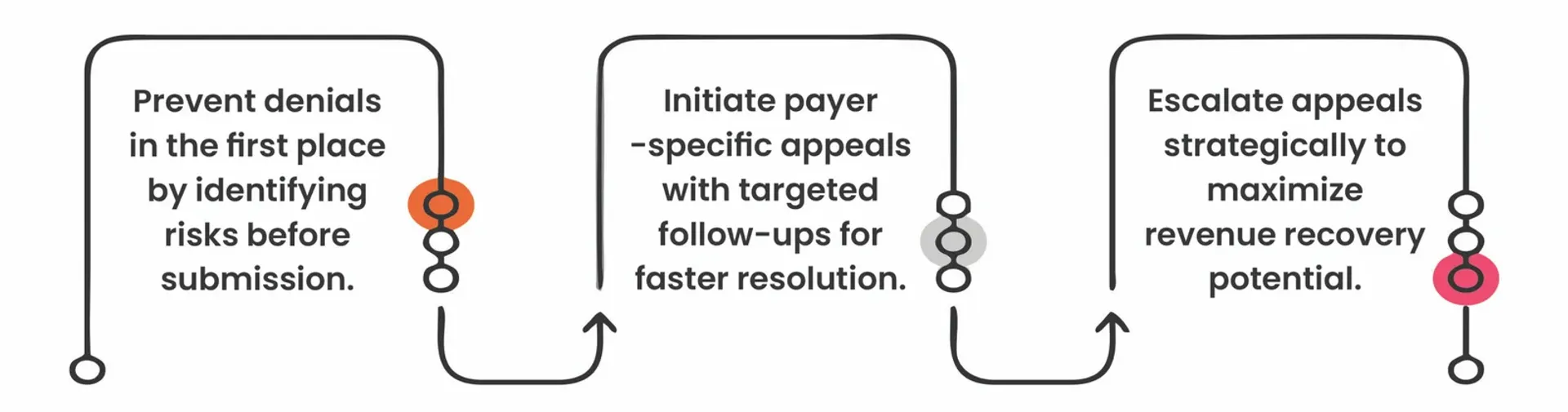
While fixing broken RCM appeals is critical, the ultimate goal should always be to prevent avoidable denials in the first place.
That’s why healthcare executives are pivoting toward prevention-first RCM strategies that combine AI foresight with expert oversight to plug revenue leaks, strengthen claims management, and reduce appeal burden altogether.
At Jindal Healthcare, our AI-powered, expert-led RCM workflows are designed to:
Why Revenue Recovery Matters More Than Ever Now
Health systems today are stretched thin and operating on razor-thin margins. Every unrealized dollar from a denied claim further limits the ability to improve collections and care.
Effective appeal management in RCM is no longer just about reclaiming revenue. It’s about restoring bottom-line balance and financial sustainability, so you can focus on what matters most.
That’s why outsourced RCM that’s AI-powered and expert-led is rapidly gaining traction as a strategic lever for sustainable revenue recovery with cost efficiency (read more on this in our eBook The ABCs 3As of Revenue Cycle Optimization).
Entrusted to an experienced partner like Jindal Healthcare, outsourced RCM can help improve your organization’s cash flow in a cost-effective, low-burden way. Because in today’s environment, no provider can really afford to leave money on the table.
Want to see how an AI-powered, expert-led RCM can help your hospital reclaim revenue faster and at a lower cost?
Connect with Jindal Healthcare’s RCM experts to explore a smarter path to AI-powered appeal management and denial prevention.
Recommended Read: The Art of Appeal: Maximizing Revenue with Appeals-First RCM