For healthcare revenue cycle management (RCM) leaders today, mastering denial management isn’t optional anymore. It’s mission-critical to their revenue maximization and organizational success. Did you know, hospitals, on average, lose up to $5 million to unresolved claim denials every year?
That’s not loose change we’re talking about—that, at times, is the difference between being able to keep the doors open and otherwise.
The good part, though, is that two-thirds of denied claims are recoverable—if worked strategically and timely. Yes, by adopting an appeals-first approach to denial management—instead of prematurely writing denials off—you can maximize your revenue, recovering money that’s rightfully yours.
Start with assessing your accounts receivable (AR) management process and building workflows to manage claim denials.
Build a Robust Denial Management Workflow
1. Start with Understanding Denials: The first step is determining the true denial reason and whether the denial is valid or not. The true denial reason can often be masked under a generic denial reason code. For instance, a medical necessity denial or a denial for service not covered may truly be a denial for an incompatible ICD.
Once you figure out the true denial reason, the next step is to assess if it needs a correction at your end. If it does, rework and resubmit it for processing.
If it can’t be corrected, you may lose the reimbursement—but it’s still worthwhile to send a courtesy appeal explaining what went wrong. This not only shows professionalism but also helps discover gaps in the existing RCM process and identify steps to prevent similar denials in the future.
2. Challenge Incorrect Denials Effectively: If the denial is unjustified, your first course of action should be to contact the payer and question the denial based on the logic and available guidelines to request the reprocessing of the claim.
If that doesn’t yield results, escalate with a focused, evidence-based appeal that considers both patient context and payer policies. A well-structured appeal strengthens your case and demonstrates due diligence in recovering revenue.
Reclaim Revenue with Strategic Appeals
Claims appeals are a formal way of contesting claims that have been denied by payers. An appeal should ideally happen when all other resolution attempts—like corrections and resubmissions—fail and you see the denial impacting your revenue and patient.
Done right, appeals can not only help you recover lost revenue but also tell you a lot about the robustness of your denial management process to get fairly compensated for your services. Moreover, when you lead with appeals, you fortify your RCM processes and payer relationships with a clearer understanding of your denials and payer needs.
Simply put, an appeals-first mindset—rather than defaulting to write-offs—can be your best weapon in healthcare RCM to reclaim revenue that rightfully belongs to you, while wielding your denial management skills with learnings from each case.
Double Down on RCM Optimization
Navigating the nuanced process of claims appeals in denial management is no walk in the park. Inefficiency in this area isn’t just a missed revenue opportunity—it can be a costly one too.
Recent industry statistics indicate that hospitals spent over $25.7 billion in 2023 contesting claims denials. This roughly translates into an additional $57 in administrative cost per claim. That’s a lot of operational burden and a compelling reason to double down on RCM optimization efforts toward preventing denials (in the first place) and resolving claims denials (with minimal efforts if they occur).
Diving into denial management with an appeals-first mindset can help you turn your RCM process into a powerhouse of healthcare revenue recovery.
Before we walk you through five strategic ways of managing denials (also best practices for appeals), let’s call out the pitfalls that often result in missed revenue opportunities for healthcare providers.
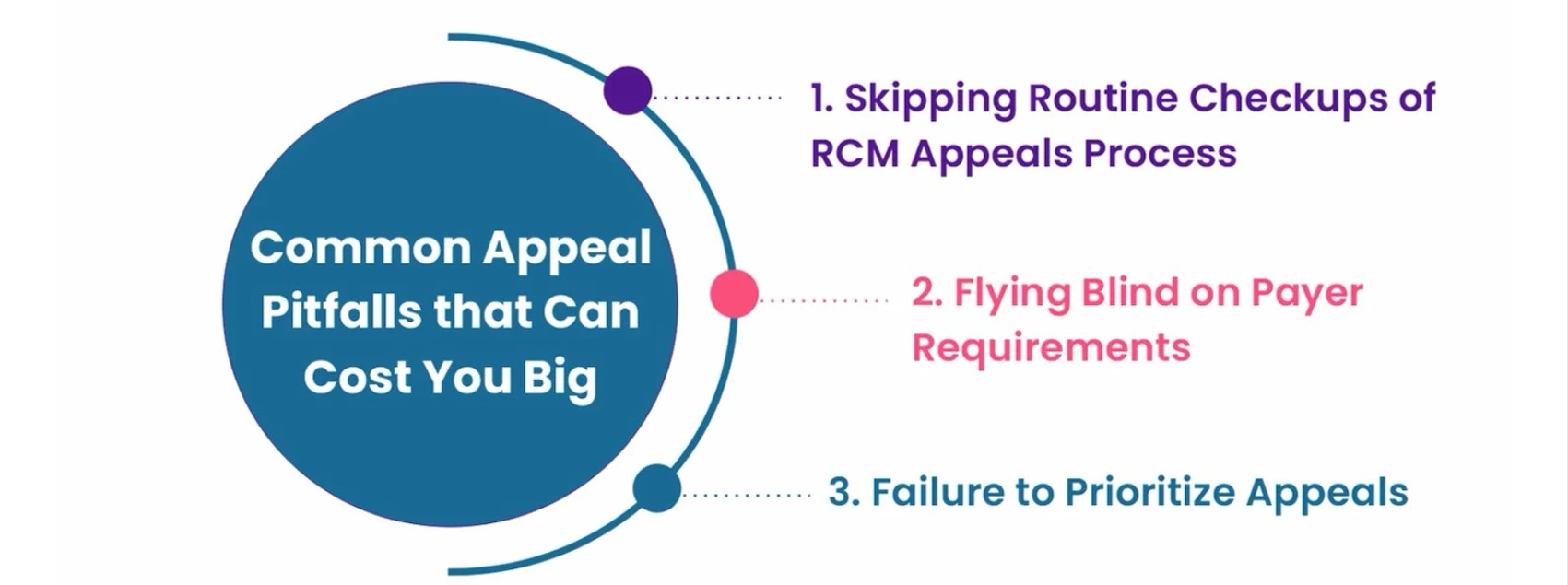
Common Appeal Pitfalls that Can Cost You Big
1. Skipping Routine Checkups of RCM Appeals Process: Healthcare organizations that fail to regularly review their appeal processes and denial management strategy despite knowing their payers’ tendency to frequently change rules often set themselves up to fall behind.
The inability to create, review, and update a documented playbook for handling appeals by payer, denial reasons, and CPT/ICD codes greatly influences appeals’ success rate. Organizations that fail to conduct this routine review often miss a pool of revenue opportunities.
2. Flying Blind on Payer Requirements: Another common mistake that providers make during the appeals process is not understanding and meeting payer requirements—and passively hoping for a Hail Mary moment that could overturn their denials.
A new KFF analysis reveals that HealthCare.gov insurers denied nearly one out of five claims submitted for in-network services and 37% of claims for out-of-network services in 2023.
Organizations that do not keep themselves abreast of payer behavior and documentation needs often find themselves struggling with the process, losing millions in revenue that could otherwise be easily reclaimed through robust appeals.
3. Failure to Prioritize Appeals: RCM teams often juggle multiple tasks in denial management without following a structured approach to resolving claim denials via appeals. Not triaging and prioritizing appeals based on their success rate or impact on their revenue cycle often results in loss of revenue.
However, with the right support of technologies like analytics and AI to review historical success rates and predict recovery rates, you can prioritize high-impact appeals to move the needle and improve your revenue cycle efficiency, realizing more revenue, faster.
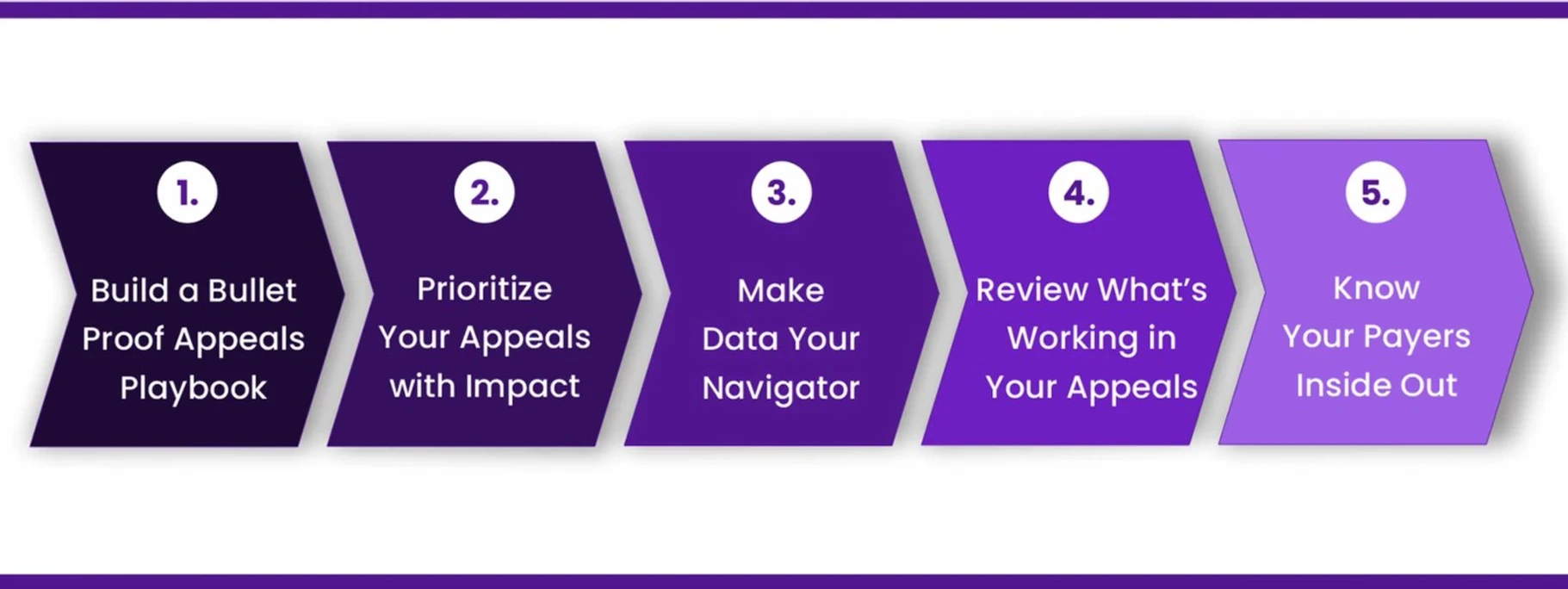
5 Effective Strategies to Strengthen Your Denial Management
1. Build a Bulletproof Appeals Playbook: Having standard operating procedures (SOPs) and appeal templates tailored to your payers and denial reasons is one of the best practices for denial management in healthcare RCM. It will not only help standardize the workflow, reducing your team’s efforts and time, but will also help you file objective, evidence-backed appeals accommodating payer needs to boost their acceptance rate.
2. Prioritize Your Appeals with Impact: While denials shouldn’t be quickly written off, not all denials are the same and worth chasing either. It’s important to understand the impact of each denial on your resources and, most importantly, your revenue cycle to prioritize appeals. Start with the low-hanging fruit—high-value, high-impact claims that can yield you more (revenue) with less (effort).
If your high-paying procedure is already paid for and a low-cost medication is bundled into it, an objective decision needs to be made to see if it’s worth the effort and risk disputing the denied code.
3. Make Data Your Navigator: While appeals to overturn denials are important to reclaim recoverable revenue, it’s equally important to understand why denials happened in the first place. Leverage AI and analytics to understand denial trends and the root causes behind recurring issues to stop them in their tracks.
These insights can also be helpful in making improvements in medical coding and billing and front-end patient access workflows—two common contributors to preventable denials.
4. Review What’s Working in Your Appeals: Regularly reviewing your appeals and their outcomes can help you assess the effectiveness of your denial management strategy and fine-tune your RCM. This will also help you understand which appeals have had a good success rate in the past and refine your approach over time. Consider these scenarios to understand the difference:
Scenario 1: We missed taking authorization for this visit but request you to reprocess the claim. Here are the medical records:
Scenario 2: We would like to request your reconsideration of this denial for missing authorization, based on the following:
- We have been treating this patient—your member—for over the past 3.5 years and have successfully submitted 19 prior claims, demonstrating our consistent adherence to your billing and authorization guidelines.
- During the visit in question, the patient required a procedure as part of their ongoing treatment plan and has since reported a 70% improvement in symptoms.
- Unfortunately, due to a one-time internal workflow lapse, we were unable to secure the authorization in advance.
- Given our longstanding relationship with your organization and your member, as well as our ongoing commitment to delivering high-quality care, we kindly request that you reconsider this denial and reprocess the claim.
5. Know Your Payers Inside Out: It’s equally important to know your payer behavior, requirements, and response to appeals. The better you know your payers, the more effective your appeal submissions will be, and the more chances will be for revenue recovery. Missing any crucial documentation requests by payers can result in missed revenue opportunities, which can eventually hurt your bottom line.
The Jindal Healthcare Advantage: People, Process, and Technology
For over a decade, we at Jindal Healthcare have been helping healthcare providers build a strong appeals process for a stronger bottom line. Our trifecta for success—our seasoned team of RCM appeal experts, SOP-driven workflows, and AI-powered technology platform HealthX—has yielded high-impact revenue cycle results for our hospital partners long struggling with poor AR and denial management.
Partnering with us for AR management services offers several advantages with a special focus on denial management and prevention with:
1. Staff Augmentation: With RCM outsourcing services, you and your team can focus back on what matters most—patient care—while our seasoned experts effectively manage your AR, driving cash flow for your financial stability.
2. Process Optimization: We ensure continuous process optimization through custom SOP and appeal template development and regular updates to keep your denial management processes and appeal workflows in tune with payer behavior and needs, thereby boosting their acceptance rates.
3. Technology Integration: We leverage the powerful capabilities of AI, automation, and analytics through our platform HealthX (read more on this in our eBook The ABCs 3As of Revenue Cycle Optimization) for RCM optimization. By analyzing denial (historical trends) with AI and intelligent dashboards, we take proactive measures to prevent their future occurrences and automate redundant manual tasks, thus boosting your RCM efficiency.
Revenue recovery is complicated, but we at Jindal Healthcare make it simpler for you. Whether you’re trying to turn the ship around, boost your appeal success rates, or get ahead of denials, our tech-enabled RCM optimization services can help you turn the tide and reclaim the revenue that’s rightfully yours.
Connect with our experts to learn how we can help you strengthen your denial management and bottom line.
Also Recommended: Claim Denials: Have You Addressed This Elephant in Your Revenue Cycle Yet?