As hospitals deliberate ways to take in the looming Medicaid changes introduced by the One Big Beautiful Bill Act (OBBBA), one thing is crystal clear: RCM readiness is more critical than ever to offset the financial impact this policy could bring.
The Act, in many ways, is poised to not just limit but also restrict access to care as a result of significant reductions in federal support for Medicaid and the Affordable Care Act. The financial blow can destabilize hospitals, compelling them to shoulder more of the burden to treat the uninsured with fewer safety nets.
OBBBA: A Beautiful Change or a Brutal Reality
At first blush, the name One Big Beautiful Bill Act (OBBBA) sounds like a picture-perfect, utopian arrangement for the US healthcare ecosystem—a promise of simplified care. But when you peel back the layers, you see a host of complexities that could leave both patients and providers with a reality far from that promise.
While the Act claims to “improve patient access,” it’s far off track in its trajectory toward achieving that goal, given the sweeping cuts it introduced in Medicaid and CHIP and the stricter eligibility criteria for access to care.
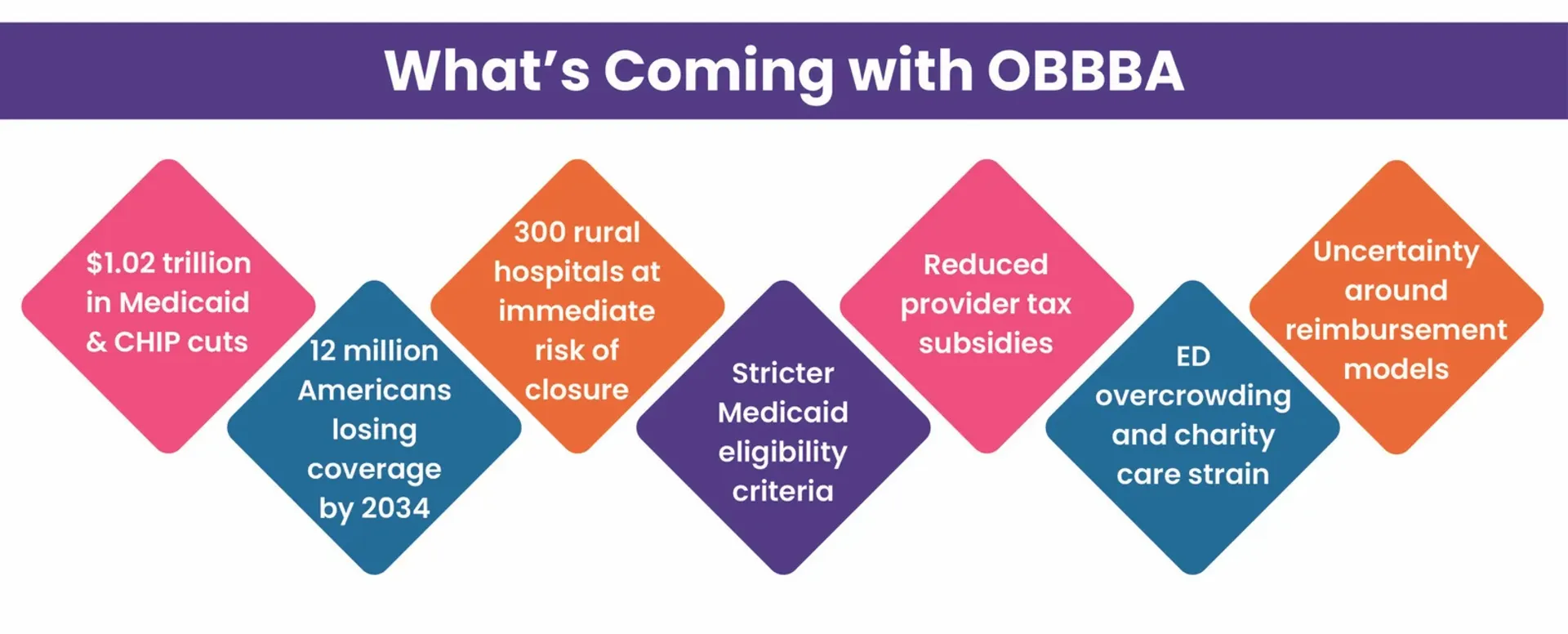
OBBBA-imposed stringent Medicaid requirements, including work mandates, shorter enrollment windows, and annual re-enrollments, can leave many Americans without coverage. And with fewer people on Medicaid, providers and hospitals will be at higher risk of receiving fewer payments as well.
With more than 12 million Americans expected to lose coverage by 2034 and over $1.02 trillion expected in Medicaid and CHIP cuts over the next decade, the pressure on healthcare revenue cycles will be unlike anything seen before—especially for rural hospitals already operating on razor-thin margins and battling for their survival.
Just a Policy or a Financial Reckoning?
OBBBA’s impact on account of more uninsured populations, more out-of-pocket expenses, and more defaults is prompting healthcare providers and RCM leaders to question their RCM readiness to survive, let alone thrive.
Ways OBBBA Can Strain Your RCM
- Care May Go Uncompensated: The OBBBA is expected to leave millions without coverage. Without coverage, patients may end up in your ED, only now without a payer backing them. This could translate to higher AR, lower collections, and more write-offs as out-of-pocket expenses soar. It remains unclear if increased reimbursement rates will make up for the lost payments physicians will face as their patients lose coverage.
- Eligibility and Authorization Complexities: New work requirements, more paperwork, and tighter re-enrolment windows will make verification and prior authorizations far more complex, requiring more detailed steps and leaving greater room for errors. All of this will have direct implications on the backend and, ultimately, on the bottom in the form of denials and higher cost to collect.
- A Double Whammy for Vulnerable Hospitals: Rural hospital providers relying heavily on state payments and Medicaid are on thin ice. Even with the Act’s proposed inclusion of a $50 billion fund over the next five years, it likely won’t offset the broader damage. With 44% rural hospitals already operating at a loss, the OBBBA could be the final push over the edge, putting more than 300 rural hospitals at immediate risk of closure.
RCM Readiness: The Need of the Hour
While the chaos triggered by this Act is inevitable, healthcare providers and RCM leaders can still lay the groundwork to bulletproof their systems, so they capture and make every dollar once the OBBBA takes effect.

How Jindal Healthcare Can Make You OBBBA-Ready
At Jindal Healthcare, we optimize and future-proof revenue cycles with our AI-enabled RCM expertise, making hospitals and health systems financially resilient. This enables them to achieve more with less, without compromising on their cash flow or care.
Here’s how we enable RCM readiness for tomorrow’s challenges:
- AI Enablement: By optimizing revenue cycles end-to-end with a thoughtful and seamless AI integration in a human-in-the-loop (HITL) RCM setup, we streamline workflows, eliminating inefficiencies and delays that impede your revenue. Think:
- AI-powered eligibility verification (via robust APIs) that enables precise patient data capture in real time from payer portals based on the exact request made, reducing your burden, unnecessary delays, and patient confusion w.r.t. cost estimates
- Flagging high-risk accounts for claim processing and financial counseling
- Prioritizing time-sensitive claims based on their ROI and historical trends
- Democratizing the best correct course of action to work claims with minimal touches.
The result: cleaner claims, timely payments, and reduced cost to collect.
- Targeted Efforts: With OBBBA in healthcare, self-pay and Medicaid denials are expected to become the norm. In such cases, your best mode of defense is to reduce preventable denials and realize your revenue potential with targeted effort.
We conduct regular denial root cause analysis and leverage our proprietary AI for AR tool HealthX Collect to prioritize and assign claims to the right expert at the right time, saving unnecessary touches and directing effort only where it’s needed. The result: fewer denials, faster turnaround, and improved collections.
- Revenue Intelligence: We dig deep into every denial to uncover and fix the root cause behind it. With the claim intelligence gathered through denial root cause analysis (RCA), we take proactive steps to prevent their future occurrence, thus reducing write-offs and rework. Our custom SOPs specific to your payer mix and nuances keep pace with payer behavior shifts and industry trends.
With robust Power BI dashboards giving real-time actionable insights into your operational workflows and RCM health, we channelize analytics in the truest sense to drive continuous process improvements with robust feedback loops. The result: data-driven RCM optimization for better financial performance.
OBBBA: A Crisis or a Catalyst for Change?
While the OBBBA introduces a financial strain for healthcare providers, it also offers an opportunity for a radical shift in the way care can be delivered and paid for. And this could just be the right time for providers to rethink their RCM readiness and take the much-needed leap toward data-intelligent, tech-enabled revenue cycles—to not just survive but thrive under the constraints this policy may bring.
Let Jindal Healthcare Get You Ready for OBBBA
At Jindal Healthcare, we equip healthcare providers and hospitals with optimized revenue cycles that work with the change and not against it. With AI-powered smart workflows and revenue intelligence, we build resilient revenue cycles that don’t just withstand policy changes but also emerge stronger.
RCM optimization journey with Jindal Healthcare begins with an expert top-down, bottom-up health assessment of your revenue cycle to uncover areas exposed to revenue leaks and risks. We then build a strategic roadmap to realize your untapped revenue potential and bring your costs down.
Connect with our experts for a strategic RCM Readiness Review to see how we can help you navigate the OBBBA shift with financial resilience and uncompromised focus on care delivery.
Recommended Read: Beyond the Numbers: How a Strategic Partner Review Helped a Texas-Based Rural Hospital Turn Data into Revenue Wins
More on OBBBA: Unpacking the OBBBA: One Bill to Touch Them All






