Historically, Traditional Medicare has been a safe haven from the red tape of prior authorization—requiring little on that front to enable seamless patient access and provider reimbursements. Prior auth complexities have largely been associated with Medicare Advantage (MA). But that’s about to change, and sooner than we expect.
Prior Authorization Isn’t Just an MA Problem Anymore
The Centers for Medicare & Medicaid Services (CMS) recently announced a major policy shift. Starting next year, prior authorization will be mandatory for certain services under Traditional Medicare, initially in six states: Arizona, New Jersey, Ohio, Oklahoma, Texas, and Washington.
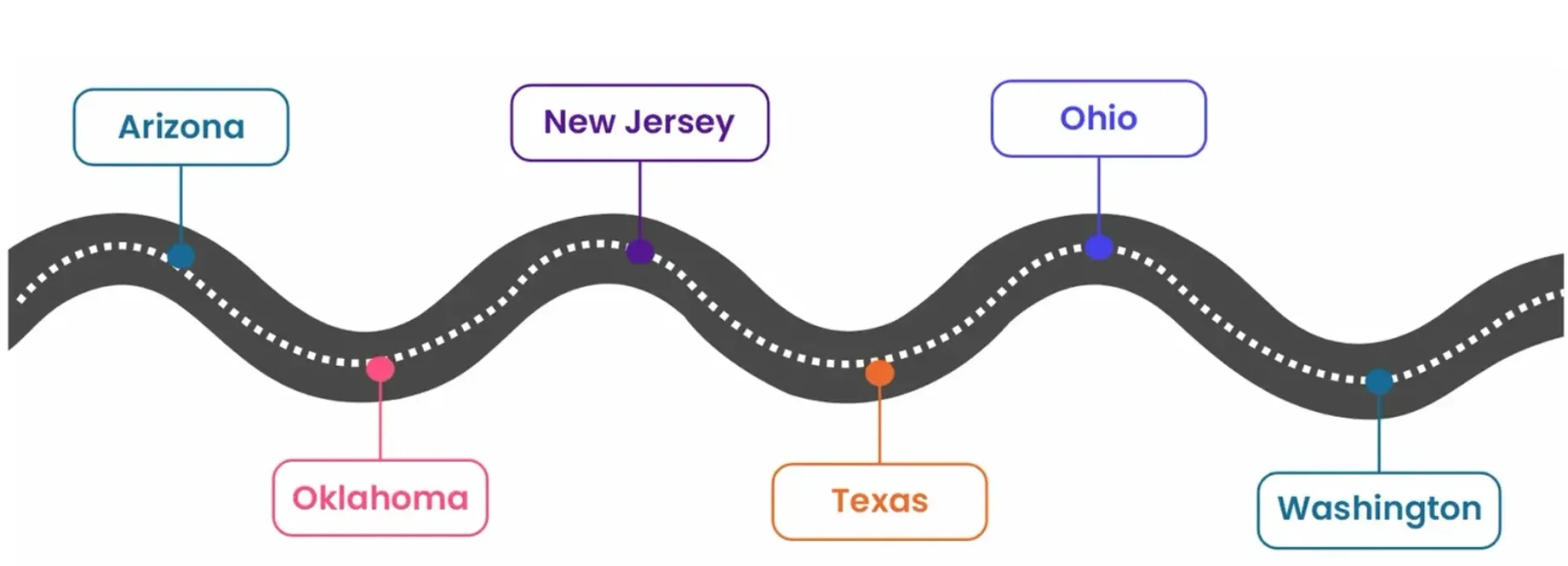
Yes, beginning January 1, 2026, prior authorization will be required for 17 services identified by CMS as vulnerable to fraud, waste, and abuse. The rollout is tied to CMS’ WISeR Model, short for Wasteful and Inappropriate Service Reduction. It will leverage AI and ML to evaluate prior authorization requests to root out waste, reduce low-value services with little to no clinical benefit, and curb inappropriate spending.
Streamlined Prior Auth or Just Another Layer of Red Tape?
Let’s talk about numbers first. According to CMS estimates, Medicare reportedly spent around $5.8 billion in 2022 on unnecessary or inappropriate services. And WISeR is positioned as its tech-driven fix to cut the waste fat, which currently accounts for 25% of US healthcare spending, with 11% coming from overuse.
It intends to apply tech-driven commercial payer-style prior authorization processes in Traditional Medicare that claim to be faster and more accurate in reducing wasteful spending.
That said, the burden of healthcare providers already grappling with administrative overload could actually increase, and here’s why.
Unlike MA plans where virtually all enrollees must obtain prior authorization for some healthcare services (over 50 million determinations in 2023 alone), Traditional Medicare currently requires far fewer reviews (under 400,000 in 2023). However, the new model could significantly increase this volume, bringing added friction and paperwork to an already stressed system.
It also raises a critical question: why add complexity to Traditional Medicare when MA is already under fire for administrative inefficiencies and delays? With the bureaucratic drag that has plagued MA plans for years getting into Traditional Medicare, here’s what healthcare providers can do to protect their revenue.
5 Moves to Future-Proof RCM Before Prior Auth Hits Traditional Medicare
Before diving in, remember—prior authorization isn’t a siloed task. For the following moves to truly work, revenue cycle-wide coordination is essential. Without seamless collaboration across the front-end (patient access), mid-cycle (coding and billing), and backend (AR and denial management) teams, even the most advanced technologies can fall short. These strategies can protect your reimbursements only when the teams are fully aligned to reduce friction.
- Audit Your Current Prior Auth Workflows: If you can’t identify your workflow gaps, you can’t improve. So, it’s critical you assess your system’s prior authorization workflows and streamline your patient access processes—from documentation to escalation—to reduce delays that can impact your patients and payments.
- Tighten and Refresh Your SOPs: Payer rules keep changing and prior authorization requirements are notoriously inconsistent. If you aren’t able to keep pace with your payers, you may have to deal with prior auth rejections and denials along the way. So, it’s important you keep a tab on your payer nuances and update your RCM playbook. This will help keep your team aligned on payer rules and documentation needs.
- Strengthen Your Front-End with Technology: Don’t shy away from leveraging technologies like AI and automation to offload high-volume front-end tasks like eligibility verification. This will not only unburden your team but also reduce human errors that eventually contribute to downstream denials that cost you expensive rework and revenue.
- Prioritize Denial Prevention over Denial Management: Most denials tied to prior authorization are avoidable if you remain proactive in your approach. Analyze past denial trends and work on improving workflows with robust feedback loops between the teams. This will help target the root cause and significantly minimize the risk of denials.
- Monitor Prior Auth KPIs to Course-Correct Fast: Regularly tracking critical prior auth KPIs like the approval rate, the appeal success rate, percentage of delayed or missing auths is one of the most effective ways of making much-needed amendments to your process. This will help reduce bottlenecks and keep your revenue on track.
How Jindal Healthcare Helps Providers Stay Ahead of Policy Shifts
The pain of prior authorization delays and denials is felt most acutely by patients and their providers, who bear the brunt of care and payment delays. As WISeR makes inroads into Traditional Medicare to change the way care is delivered and reimbursed, healthcare providers must ensure their RCM readiness.
With trusted AI-powered RCM expertise, we, at Jindal Healthcare, help providers streamline their prior authorization workflows by doing the heavy lifting, so they can stay focused on patient care:
- Custom SOPs Built as per Your Payer Nuances: We build and update SOPs specific to your organization and payer mix. This helps reduce rework and improve first-pass success by ensuring your prior authorization requests are accurate, complete, and check all payer boxes to fast-track approvals and reimbursements.
- AI Meets Human Expertise: Our proprietary AI platform, HealthX, delivers clean, structured, and contextual data for each claim. This allows our RCM experts to work with precision, resolve issues early with AI support, and improve processes, enabling quicker approvals and faster payouts.
- Proactive Denial Prevention: By combining AI with experienced oversight, we proactively prevent prior auth denials that lead to revenue loss. HealthX offers precise contextual data for every claim to help our experts get to the root cause of prior authorization denials to plug revenue leaks, prevent future downstream denials, and supercharge revenue.
Don’t Wait Until 2026 to Act
While there’s time for prior authorization to hit Traditional Medicare, the writing is on the wall. And this is the time to make your revenue cycle resilient and future-proof to avoid getting caught off guard.
Contact our experts today to learn how Jindal Healthcare can help you turn this policy shift into a strategic enabler to meet your RCM potential.