As healthcare systems continue to feel the pinch of staffing shortages, policy shifts, and ever-changing payer dynamics, all while losing millions to claim denials every year, the call to do more with less couldn’t be clearer.
And these numbers don’t just speak facts; they underscore the urgency to act:
- 15% of initial claims denied for payment in 2023, up from 9% in 2016
- More than 39 prior authorizations handled by physicians every week
- Over $200 billion spent annually on healthcare administrative tasks
Why Revenue Cycle Management Is Primed for a Tech Leap
Healthcare is a high-stakes industry, with practically no room for inefficiency in any of its lines of work—including, revenue cycle management (RCM).
Yet, many healthcare providers wrestle with RCM inefficiencies like incorrect eligibility checks, inaccurate charge capture and documentation, and delayed AR follow-ups, which impact their margins and patient experience.
Sure, AI has made enough noise already in healthcare RCM, but a lot of what’s called “AI” out there barely scratches the surface. Most tools often fall short of unlocking your billing system’s true revenue potential through end-to-end RCM optimization.
That’s where Agentic AI changes the game!
But before diving into what Agentic AI is and what it does to your RCM, let’s first briefly discuss a few tech-driven use cases in RCM and why these technologies aren’t necessarily truly AI.
Not All “AI” Is Created Equal
A lot gets bundled under “AI” that isn’t necessarily AI. While it’s become a catch-all for these technologies, here’s the broader tech spectrum and where Agentic AI sits on it in RCM:
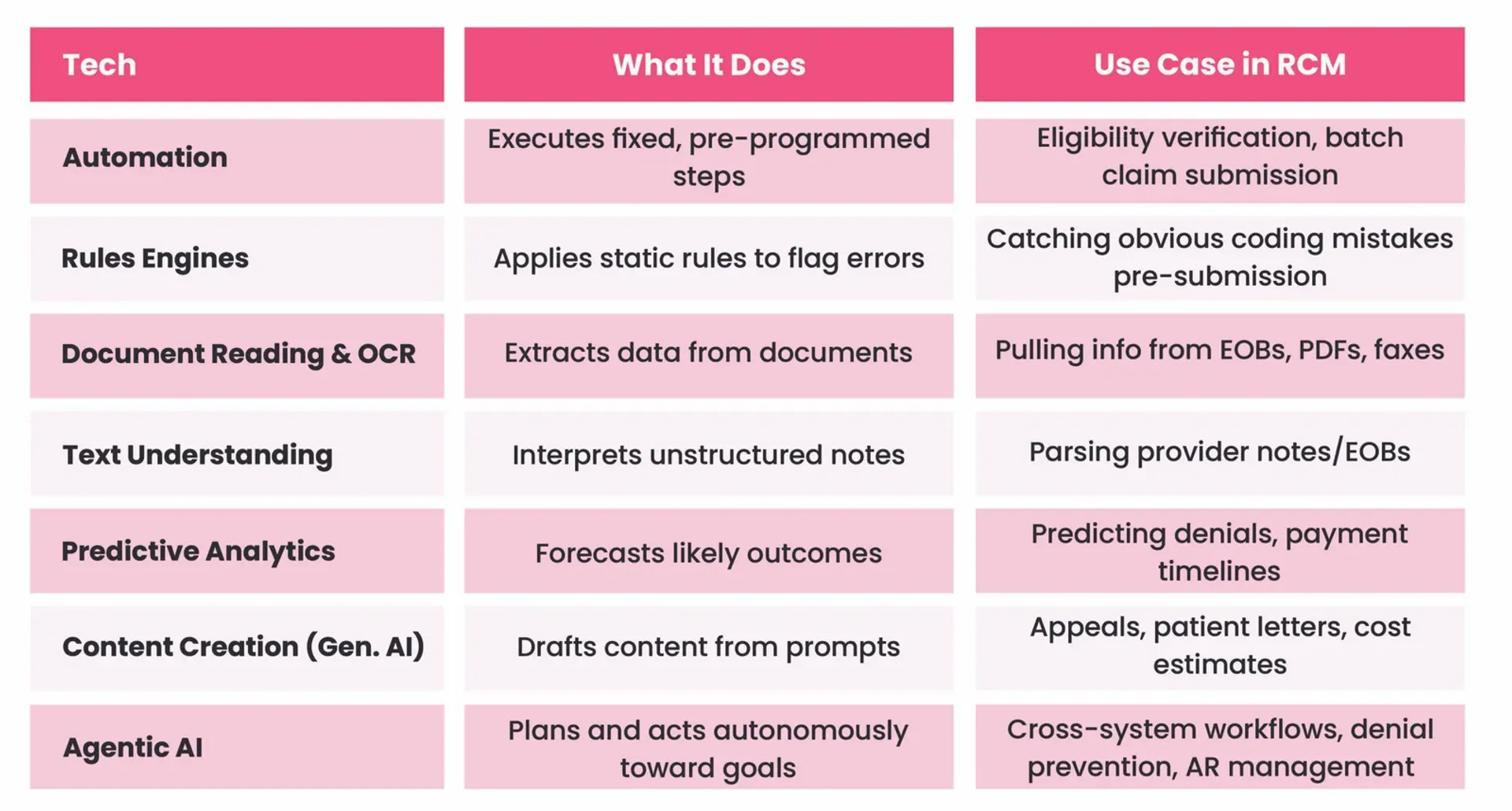
While all these have their own place in RCM, the industry is steadily moving toward something that’s autonomous, adaptive, and analytics- and outcome–driven: Agentic AI.
What’s Agentic AI and What Makes It a Game-Changer?
Agentic AI is a next-generation autonomous intelligent platform capable of thinking, reasoning, and taking actions to deliver outcomes—without constant oversight.
Think of it as the smartest teammate you’ve ever had, one that gets things done without any handholding.
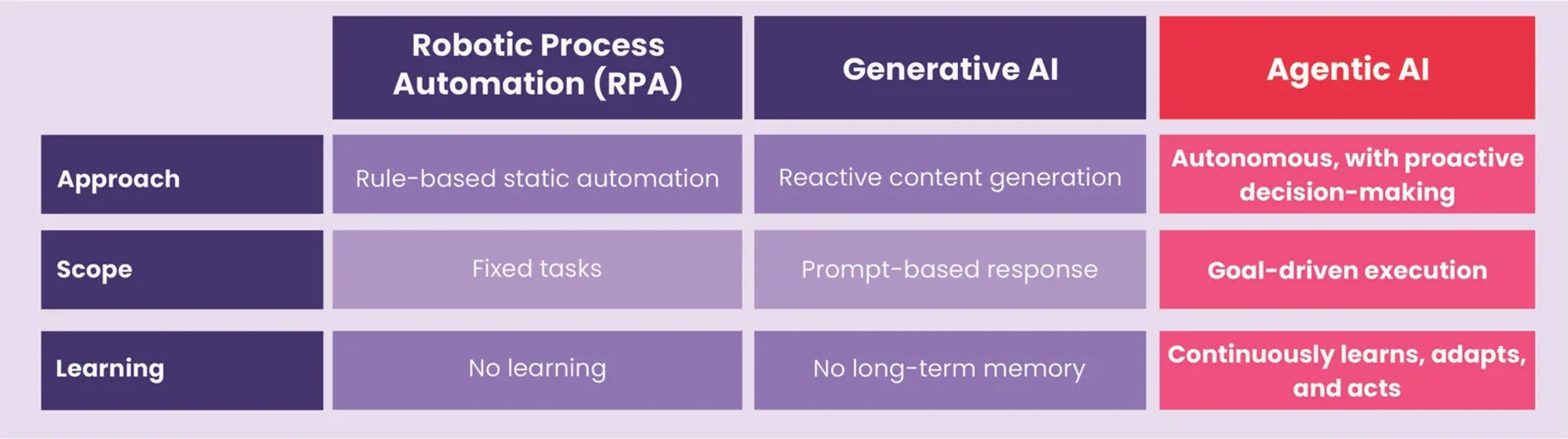
Unlike robotic process automation (RPA) bots that follow pre-defined rules or Generative AI tools (think ChatGPT) that create prompt-based responses, Agentic AI thinks through real-world complexities and proactively executes actions, just like a human would.
Quick Comparison:
Why Healthcare RCM Is Ripe for Agentic AI Intervention
The inherent complexities in RCM, from patient access to billing and AR management, create an optimal environment for intelligent intervention with Agentic AI.
While RPA bots focus on minimizing human effort on mundane tasks, Agentic AI can actually fix RCM systemic inefficiencies by:
- Interpreting data and submitting cleaner claims the first time
- Automating complex, multi-step RCM workflows end-to-end
- Adapting to payer rule or portal changes without reprogramming
- Coordinating actions across multiple systems in one flow
- Freeing up staff to focus on edge cases and high-value tasks
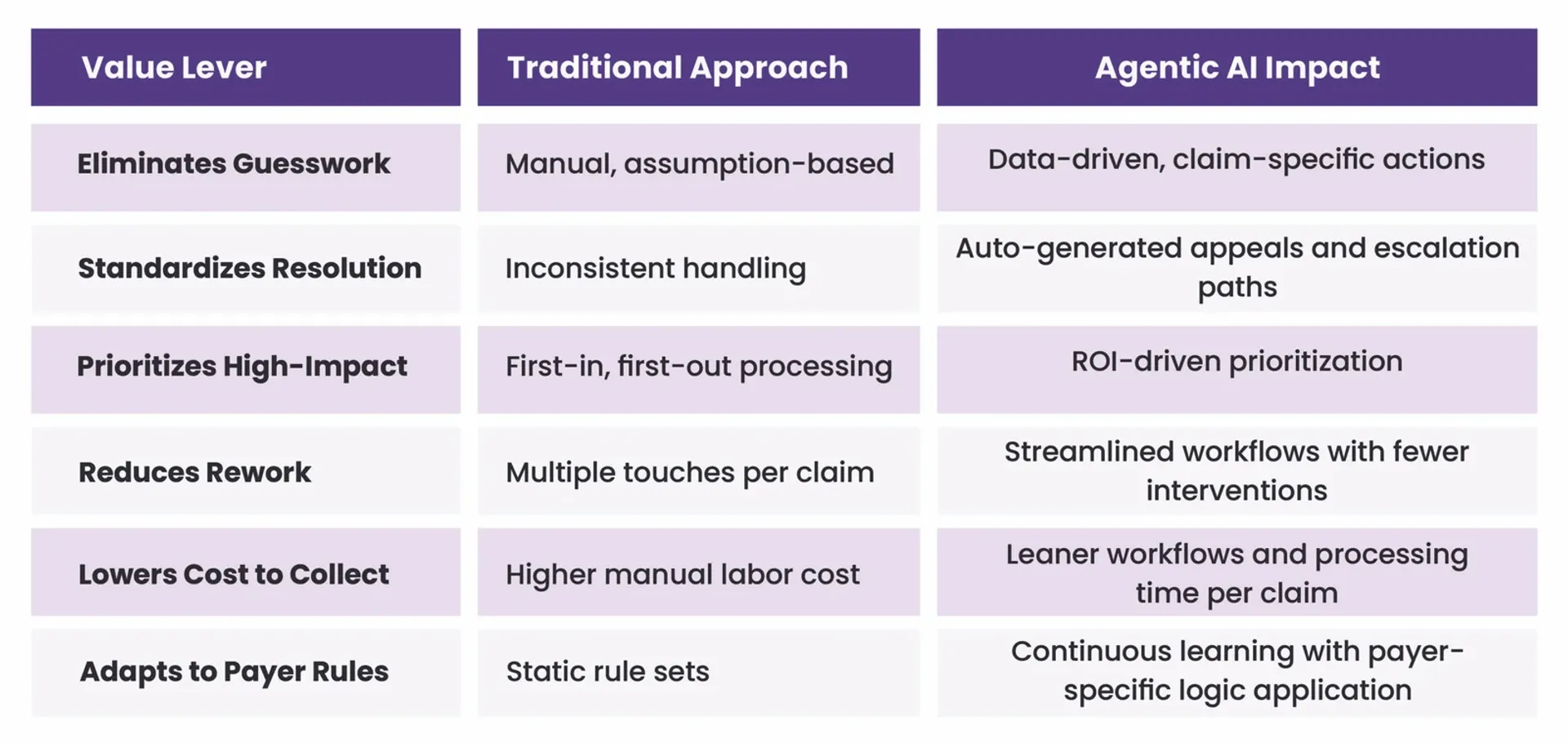
Built for Intelligent Execution, Not Merely Automation
Unlike other tools and technologies that barely scratch the surface with automation, Agentic AI dives deeper. It feeds on clean, structured, contextual data to work claims—without guesswork, without handoffs, without burnout.
It doesn’t just automate, it thinks before it acts—learning from each claim and executing the next best course of action to resolve claims faster with leaner workflows.
Capabilities Include:
- Complex Task Execution: Autonomously manages prior authorization and eligibility verification, CPT/ICD-10 coding complexities, and denial management
- Workflow Optimization: Orchestrates workflows end-to-end, cutting down administrative clutter
- ROI-Based Claim Prioritization: Prioritizes and works claims based on ROI, impact, and age, eliminating touches that inflate cost to collect
- Contextual Guidance: Offers the next best move for every claim based on its history and scenario
- Root Cause Analysis: Goes beyond flagging errors to prevent future denials
- Appeal Generation: Creates payer-specific appeals with proven success patterns
- Smart Escalation: Determines optimal escalation paths and timing with built-in logic
- Continuous Learning: Learns from every claim to improve performance, creating a continuously optimizing revenue cycle that gets smarter over time
By bringing claim intelligence and decision-making capabilities to RCM, Agentic AI acts as a co-pilot that seamlessly navigates complexities, eliminates operational turbulence, and ensures a smoother path toward accelerated cash flow.
Does More Than Just Answering
Agentic AI in RCM does more than just answering. It’s capable of bringing about a real change in your revenue cycle. With smart escalation, auto-document generation, and contextual guidance, you always know the best next move for your claim.
- Patient Access: Automated eligibility checks, prior authorization management
- Medical Coding: Handling of complex CPT/ICD-10 coding and billing logic
- AR and Denials: Payer-specific escalation, autonomous appeals, denial prevention
Whether it’s comprehensive eligibility checks for streamlined patient access or tailored appeal generation for denial resolution, it can accomplish RCM tasks intelligently and autonomously, empowering you to stay focused on patient care.
Value Levers: How Agentic AI Transforms RCM Performance
Jindal Healthcare’s Bold Bet on Agentic AI
At Jindal Healthcare, we’re not just watching the future—we’re building it.
And Agentic AI is our bold leap into the future of RCM to deliver critical capabilities that help:
- Enhance process efficiency via continuous learning
- Resolve claims faster with leaner workflows
- Intelligently prioritize and automate complex tasks
- Accelerate collections with lower operational costs
- Built revenue cycles that adapt and improve continuously

Jindal Healthcare’s Agentic AI brings together these three pillars to create an RCM system that’s revenue-focused and future-ready.
Ready to Witness It in Action?
With an Agentic AI powered by purpose and built for continuous learning, we, at Jindal Healthcare, are paving the path for intelligent, resilient, future-ready revenue cycles to enable healthcare providers to do more with less by:
- Bringing contextual intelligence to every claim to keep their revenue on course
- Going beyond surface-level automation to work complex tasks with precision
- Driving cost-efficiency at scale without burning out the team or adding FTEs
- Leveraging smart decision trees to minimize costly touchpoints, reduce costs
Schedule a free expert consultation today and discover how Jindal Healthcare can help you unlock your true revenue potential with its AI suite for end-to-end RCM.