Medical billing denials is the biggest stumbling stone in the healthcare revenue cycle. As per Etactics, “In 2021, there were 48.3 million denied claims, accounting for 16.6% of all claims submitted that year.” There can be multiple reasons behind rising claim denials in a practice. Some of these are manual paperwork, medical billing, and coding errors and input omissions. Another major aspect that often incites more denials than you realize is missing submission deadlines. Keeping track of each of these factors is crucial to ensure a practice maintains a healthy clean claims ratio and improved net collection rate.
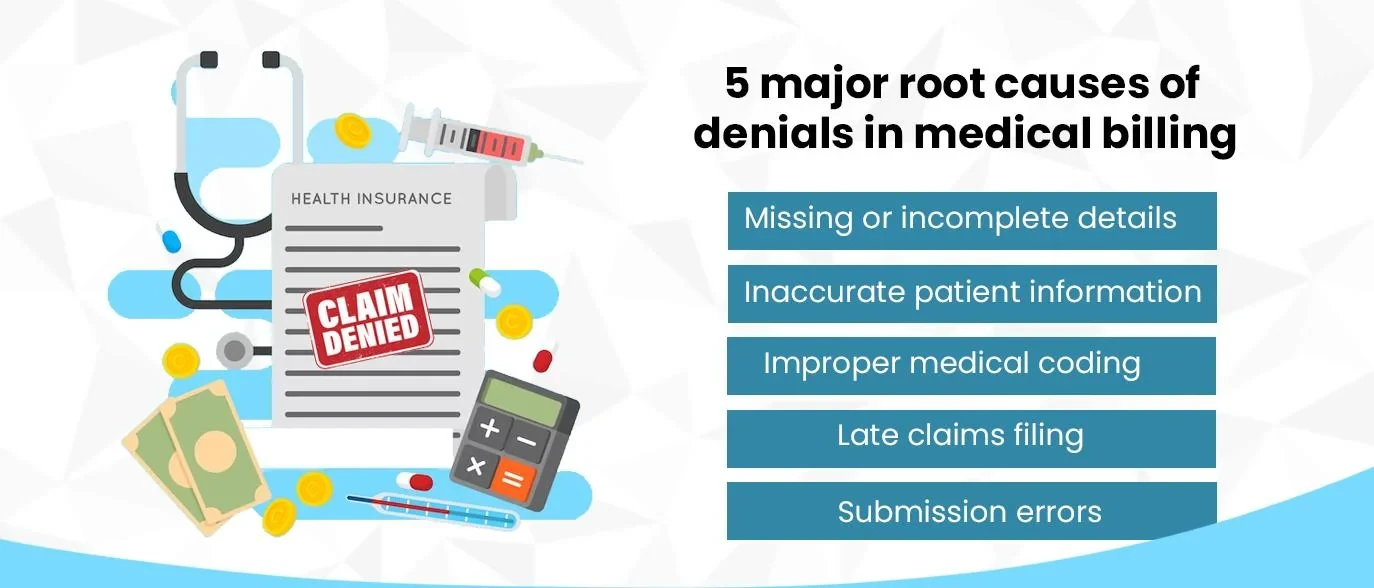
5 Major Root Causes of Denials in Medical Billing
When a claim gets denied, it not only affects the financial health of the practice but also impacts the patient’s experience. Let’s study why medical claims are denied by insurance payers.

Missing or Incomplete Details
Leaving blanks in claims form or submitting incomplete details with missing details of social security numbers, modifiers, plan codes, and demographic/technical details results in claims denial. To avoid denials in medical billing, practices need to ensure that the claims submitted are properly documented and required fields are filled.
For example, a patient visited your facility to report osteoporosis. Your administrative team provided great patient access like creating the account and automating scheduling. So did the doctor by providing the best possible value care and writing prescriptions. And at the time of filing claims for the services rendered with the patient’s insurance provider, BCBS, your team ended up missing a few critical details. It could translate to increased A/R days and denials.
Inaccurate Patient Information
On receiving a claim, providers need to thoroughly cross-check the patient’s name, gender, and birth date with the information provided by the insurance payer. This helps ensure that the final claim submitted is correct. Most often, manual claims processes result in such types of denials. The entire process takes up a lot of time when done manually and hence an automated system needs to be in place.
Improper Medical Coding
Medical coding is how practice turns the services provided into billable revenue and any coding errors have the potential to hamper the practice’s revenue. According to the Center for Medicare and Medicaid Services, 30% of claims are either denied, lost, or ignored due to minor medical billing and coding errors. The use of outdated coding books, either CPT, ICD-10 or HCPCS and/or super bills will result in delayed or denied claims and loss of revenue.

Late Claims Filing
Claims are often denied due to missed submission dates, and deadlines. This could be a result of missed or overlooked filing dates and manual processes because the claims management team gets occupied with the filing works and they fall behind in processing and submitting claims on time. An automated revenue cycle management solution can set batches for claims submission that will free up time for billers to focus on high-ROI tasks.
Submission Errors
Besides the major errors, even some small mistakes such as misspelled names or typos at the billing staff’s end can sometimes cause claim denials. This often happens when medical staff has to fill and submit the claims manually with other tasks to be performed simultaneously. The right RCM solution can help practices automate these tasks and advance fewer denials, higher clean claims rates, and accelerated reimbursements.
6 Practices to Reduce Medical Billing Denials
A steady flow of revenue is required for successful medical practice to sustain business and growth. Perhaps, part of that is ensuring accurate medical billing that could not cause any damage to the bottom line. Here are 6 tips for practices to avoid medical billing denials:
a.) Implementing robust patient registration processes to ensure accurate patient information
b.) Regular staff training on coding practices and payer requirements
c.) Using coding software to assist with coding and documentation
d.) Maintaining comprehensive documentation to support medical necessity
e.) Using electronic claim submission tools and tracking claim submission deadlines
f.) Following up with payers as needed to ensure timely claims processing
Implementing these strategies, healthcare providers can reduce the likelihood of medical billing denials and ensure steady revenue streams.

Role of Technology in Reducing Denials – HealthX 2.0
Technology can play a significant role in reducing medical billing denials. Electronic health records (EHRs) can help healthcare providers maintain comprehensive patient records and support accurate medical coding and documentation digitally without relying on paperwork. EHR allows quick access to patient records helping practices deliver quality care and health analytics that help recognize patterns, predict diagnosis, and suggest potential treatment options. Despite the enormous data available at the practice’s dispense, they find it hard to improve patient access, provide value-care delivery, and accelerate reimbursements. This is where an end-to-end Revenue Cycle Management (RCM) partner can bring transformative changes to practice.
We, at Jindal Healthcare, leverage our AI-based proprietary tool, HealthX 2.0 to analyze the practice’s EHR and automate revenue cycle processes. This analytical data is presented through result-centric operational flows using Power BI that help identify easy claims and reduce medical billing and coding errors, prioritize claims, accelerate revenue, minimize denial rates, and improve claims submission efficacy.
Bottom Line
Medical billing denials can have a significant impact on healthcare providers, both financially and operationally. However, by understanding the root causes of denials and implementing strategies to reduce them, healthcare providers can ensure steady revenue streams and improve patient satisfaction. Medical practices can reduce denials by implementing robust patient registration processes, regular staff training, using coding software and electronic claim submission tools, and following up with payers as needed. Denials can lead to significant financial losses for healthcare organizations, and the root causes of denials can be complicated and difficult to address. EHRs and revenue cycle management software can also play a significant role in reducing denials and improving revenue cycle. By taking a proactive approach to medical billing, healthcare providers can ensure that they are maximizing revenue while providing high-quality care to their patients.