Why DME Providers Can’t Risk Going Into January 2026 Without AI Eligibility Verification
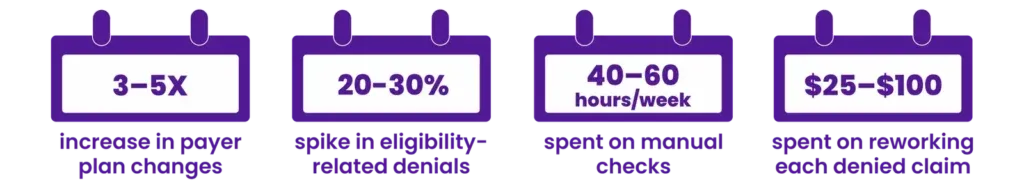
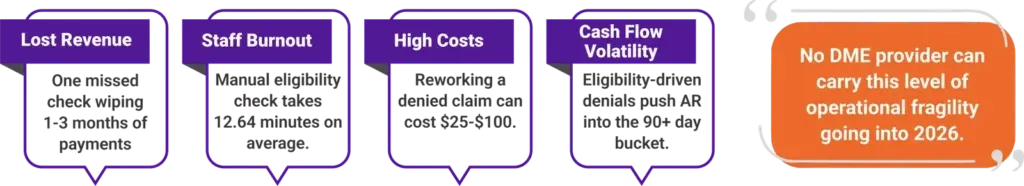
The Data Is Telling: Manual Eligibility Is Breaking DME Revenue Cycles
Open Enrollment isn’t just a seasonal eligibility reset. It’s a window that determines how predictable (or vulnerable) your revenue will be next year.
The #1 Mistake DME Providers Make Every January
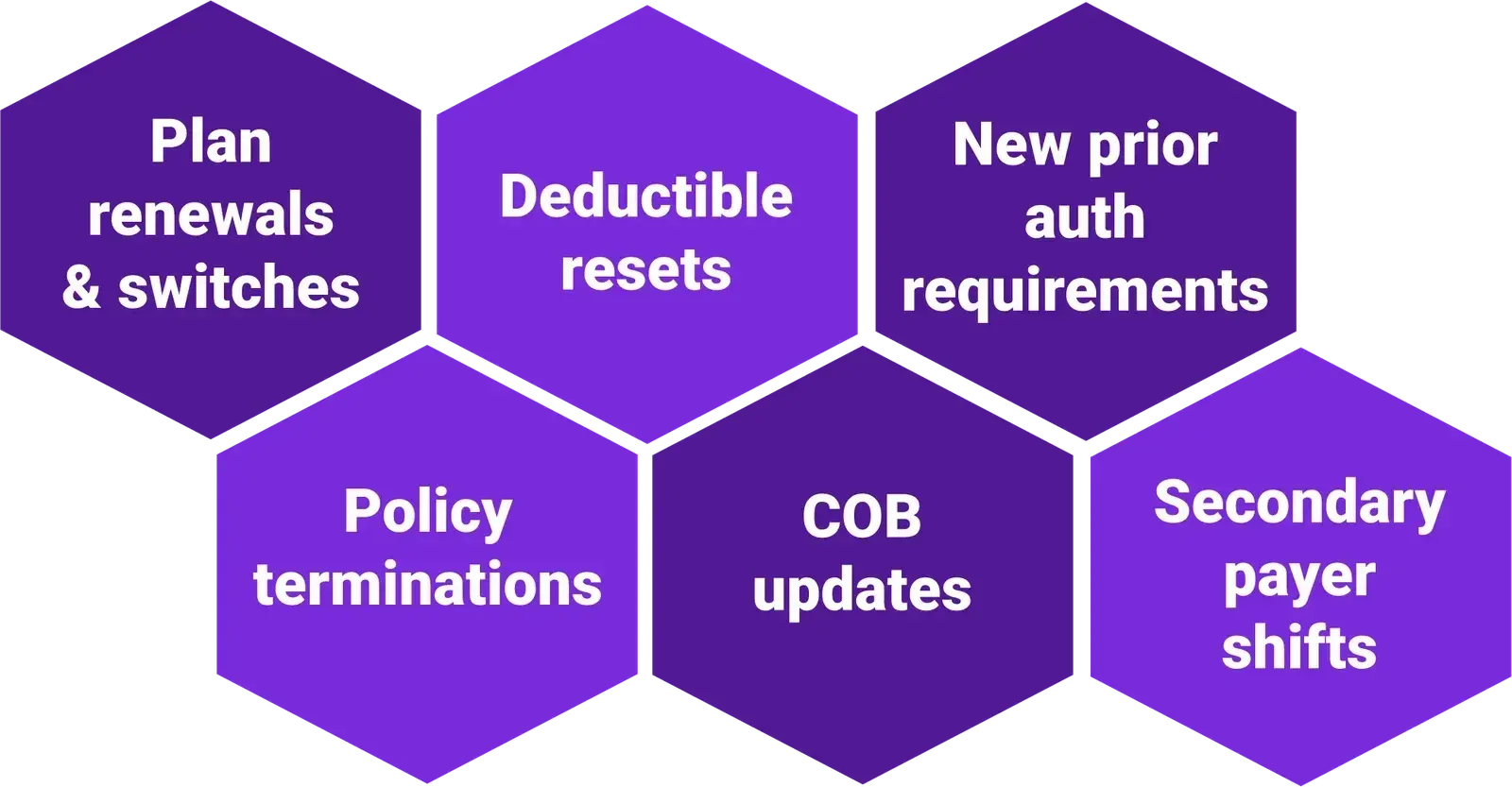
Open Enrollment resets the very rules your revenue depends on:
Yet most DME providers continue billing using last month’s eligibility data, and that’s where the bleeding starts:
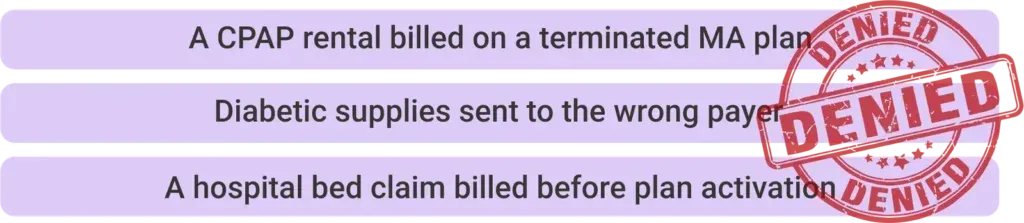
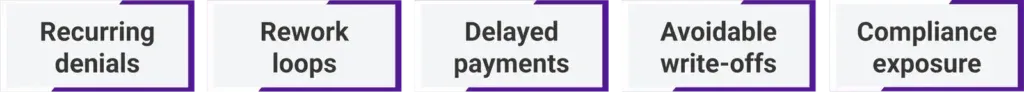
When eligibility isn’t verified every cycle, you’re bound to stare down:
And by the time your team backtracks the root cause, you’ve already lost the billing cycle and possibly your revenue too.
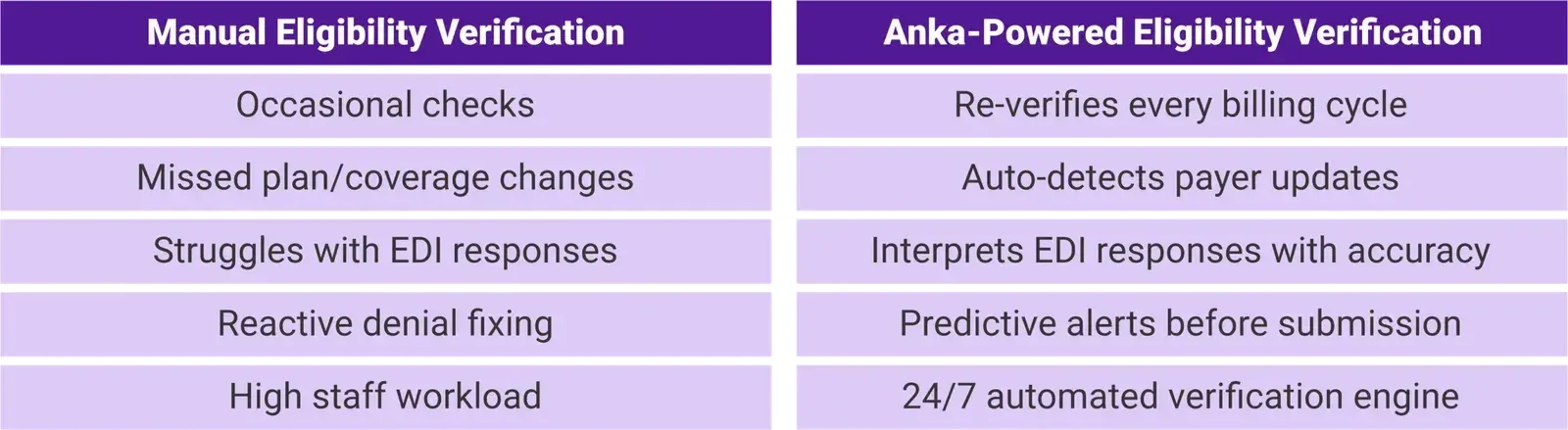
Manual Eligibility Verification Can’t Keep Up. Not Anymore.
AI Eligibility Verification: The Shift DME Providers Must Make Now
And this is exactly where Anka comes into the picture—pushing AI's boundaries to autonomously carry eligibility verification end-to-end.
Meet Anka
Jindal Healthcare’s Agentic AI Built to Protect DME Revenue Every Cycle
Anka is engineered for the real-world chaos DME providers face during Open Enrollment and beyond.
It is a purpose-built AI eligibility verification solution that verifies eligibility in real time, tracks payer shifts, and updates your workflows, proactively preventing denials and protecting your revenue.
What Makes Anka a Game-Changer in Eligibility Verification
Why DMEs Reliant on Manual Verification Need AI More Than Ever
The Most Important Move DMEs Must Make Before January 2026
Open Enrollment isn't just a busy quarter in healthcare; it’s a financial game-changer for those who adapt and evolve to lead with confidence.
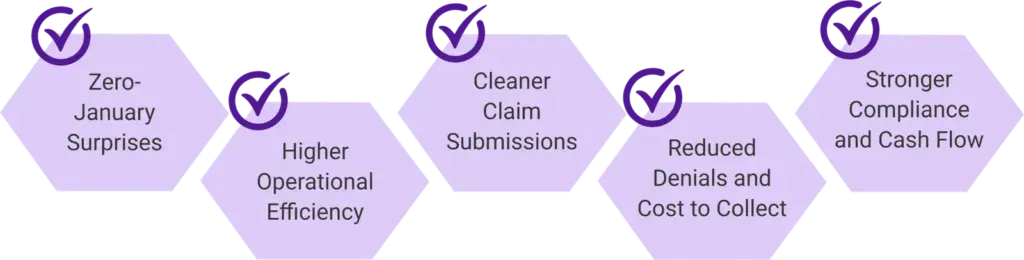
Smart DME providers are already pivoting to AI with Anka to lead 2026 with: